Left Ventricular Function
Assessment of LV systolic function is a central part of the evaluation of cardiac disease. LV function is important for guiding patient management and prognosis, and it is essential in the evaluation of patients with known or suspected cardiac disease. There is a close relationship between declining LV function and poor prognosis. This relationship is related to the degree of LV systolic dysfunction. LV systolic dysfunction following a myocardial infarction is associated with a 2.4- fold increase in the relative risk of death. Greater degrees of LV systolic dysfunction is associated with a worse prognosis. Survival of patients with an EF of less than 35% is 21% at 12-years and 54% for those with an LVEF of 35% to 49%. Both survival rates were markedly worse than that of patients with normal LV systolic function. Numerous methods can be used in LV assessment from very simple linear techniques (which are no longer recommended by current guidelines) to the more complex 3D models which are out of the scope of the Focused Cardiac (FoCUS) component of POCUS.
The essence of FoCUS is mainly a dichotomous interpretation of the findings to answer questions that are crucial to the clinical decision-making process. The diagnostic approach of FoCUS is qualitative or semiquantitative and the examination is conducted without the requirement of performing specific measurements. We will explore some qualitative appreciation of sizes and function of the LV and go slightly beyond this scope and explore some popular easy to use quantitative assessments and remind you of their limitations. This is so that you have several tools to use depending on your ultrasound's capability.
1. Visual Global Assessment
The objectives of FoCUS is to be qualitatively evaluate a LV that is dilated or non dilated, hypertrophic, hypokinetic and a function that is hyperdynamic, depressed or severely depressed. As it turns out, visual estimations of global function approximate formal quantitative methods in trained observers and we will use this to our advantage by comparing the different ranges and we will use the parasternal short axis view and apical 4 chamber view for comparison purposes.
2. Biplane disk summation (beyond FoCUS)
Lets now move beyond the scope of a Focused cardiac exam and look at the current recommendations for estimation of LV EF. Volume measurements are usually based on tracings of the blood-tissue interface between compacted myocardium in the apical four- and two-chamber views and. At the mitral valve level, the contour is closed by connecting the two opposite sections of the mitral ring with a straight line. LV length is defined as the distance between the middle of this line and the most distant point of the LV contour. This method corrects for shape distortions and uses less geometrical assumptions compared to linear models (seen next). Ultrasound machines may have this feature built in.



1
2
3
LV EF calculation by Simpson's method. 1 is a still image at end diastole on the apical 4 chamber view. 2 is a still image on the same view but at end systole. 3 is a still image at end systole and its companion at end diastole is not displayed. LV EF is thus calculated LVEF= (LVED-LVES)/LVED.
3. Linear Dimensions to Estimate EF
Linear dimensions to assess of LV function can be done with with M-mode or 2-dimensional (2-D) echocardiography and are performed in the parasternal long- and short-axis views. Change in LV cavity dimensions during systole can be used to calculate LV fractional shortening and ejection fraction. The major limitation of these techniques occurs in patients with regional LV dysfunction because assessment of ventricular systolic function in 2 opposing basal segments is unlikely to provide an accurate reflection of overall LV function. Inaccuracies can also result from the geometric assumptions used to calculate LVEF from linear ventricular dimensions. In addition, cardiac orientation often results in difficulties in attaining perpendicular alignment of the M-mode beam with the LV long axis Hence, current echocardiographic guidelines no longer recommend using linear measurements to calculate LVEF.
3A. Fractional Area Change
Fractional area change (FAC) is a measurement technique on 2D ultrasound and used on the Parasternal short axis view at the mid-papillary level. It measures the change in area that happens in systole and diastole and is used as a surrogate for Ejection Fraction but FAC is not EF. EF is based upon volume as opposed to FAC which is based on area. Clearly this linear technique has a number of assumptions on the geometry of the ventricle and overall LV function. FAC is more accurate than fractional shortening (see below) since we are looking at all wall segments (six of them on this view) as compared to 2 segments (fractional shortening). This measurement is highly preload and afterload dependent. .

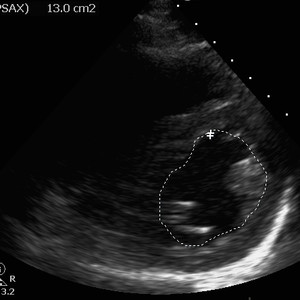
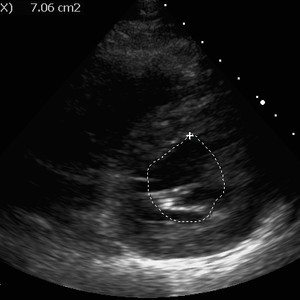
1
2
3
FAC estimation. On clip 1, short axis mid papillary view. D marks the end of diastole, S marks the end of systole. Still images 2 and 3 represent end diastolic and end systolic areas respectively.
FAC is calculated in the images above. The ultrasound machine can go frame by frame into the past once images have been recorded into the ultrasound machine. Then you can trace back the moment the ventricle has the largest area marking end diastole (D markings on the upper left image) and tracing can occur at that level (middle image). Then the smallest area is traced marking end systole (S marking on the upper left image and right image).
FAC is calculated as FAC=(End Diastolic Area - End Systolic Area)/ End Diastolic Area
A normal value is considered >40% and severe LV systolic dysfunction is considered when this value is <20%
3B. Fractional Shortening
By using M mode on the parasternal short axis view we have can make very accurate assessments on the timing on the structures interrogated by the scan line. Since we are only using 2 opposing walls on this measure we are making several assumptions. Ventricular internal dimensions are measured from leading edge to leading edge as shown in the following images:


1
2
LV
RV
Fractional shortening estimation. Clip 1 shows the scan line bisecting the papillary muscles. Still image 2 shows the M mode of that scan line over time. LV, left ventricle; RV right ventricle.
M mode scan line shown on the left hand image. The M mode feature is turned on and then is frozen to interrogate the scan on the right hand side image. The red line indicates end diastole and green, end systole.
A normal range is 25-45%
This method was widely used previously but M-mode linear measurements of LV function are problematic when there is a marked regional dysfunction. Keep in mid that an oblique internal diameter will lead to errors in length measurements.
3C. E-Point Septal Separation
E-Point Septal Separation (EPSS) can be used to determine when a patient has severe LV dysfunction. By using M mode on the parasternal long axis view we have can make very accurate assessments on the timing on the structures interrogated by the scan line. This time, we are looking at the distance between the anterior mitral valve leaflet and the LV septum on diastole and it is the closest distance they are from each other.



E point
A point
Septum
Mitral valve
1
2
3
E-point septal separation. In clip 1, long axis view. Notice on this clip that the anterior mitral valve is touching the interventricular septum and it is what we can appreciate in still image 2. The EPSS is essentially 0 here. On still image 3, we can appreciate that the anterior mitral valve struggles to get to the septum.
The M mode scan line is placed over the tips of the MV and then the M function is then turned on (middle image). The anterior mitral valve waveform on M mode contains 2 peaks. The first is the E-point and corresponds to the maximal mitral valve opening in early LV diastole. The second, smaller peak is called the "A-point" and corresponds to atrial contraction later in LV diastole. Typically the mitral valve should open with the leaflet hitting or coming very near to the interventricular septum at the E-point. The longer this distance, the worse the EF.
A EPSS >7mm corresponds to a reduced LVEF and a value >13mm indicates severely reduced LV dysfunction.
References
1. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1-39.e14.
2. Via G, Hussain A, Wells M, Reardon R, ElBarbary M, Noble VE, Tsung JW, Neskovic AN, Price S, Oren-Grinberg A, Liteplo A, Cordioli R, Naqvi N, Rola P, Poelaert J, Guliĉ TG, Sloth E, Labovitz A, Kimura B, Breitkreutz R, Masani N, Bowra J, Talmor D, Guarracino F, Goudie A, Xiaoting W, Chawla R, Galderisi M, Blaivas M, Petrovic T, Storti E, Neri L, Melniker L; International Liaison Committee on Focused Cardiac UltraSound (ILC-FoCUS); International Conference on Focused Cardiac UltraSound (IC-FoCUS). International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr. 2014 Jul;27(7):683.e1-683.e33. doi: 10.1016/j.echo.2014.05.001. PMID: 24951446.
3. Gudmundsson P, Rydberg E, Winter R, Willenheimer R. Visually estimated left ventricular ejection fraction by echocardiography is closely correlated with formal quantitative methods. International Journal of Cardiology,
2005; Vol 101: Issue 2: 209-212. ISSN 0167-5273.










